How to Tell If Your Loved One is in Pain: 7 Caregiver Tips That Really Work
Pain doesn’t always announce itself. Sometimes it’s obvious — a grimace, a sharp cry, a hand clutching the belly. Other times, it hides in silence, in skipped meals, or in restless tossing at night.
If you’re a caregiver, you already know: your job isn’t to magically erase pain. It’s to notice it early, ease what you can, and know when to call in extra help. That’s why learning how to tell if your loved one is in pain is one of the most important skills you can develop.
Why Pain Often Goes Unspoken
The Silent Struggle of Pain
Not everyone is quick to say, “I hurt.” For some, admitting pain feels like weakness. Others downplay it to avoid “being a burden.” And some simply can’t express it — whether because of illness, memory loss, or fear of what the pain might mean.
Why Caregivers Become Detectives
That’s where you step in. Caregiving is detective work. You’re watching for clues — facial expressions, small sounds, or tiny shifts in routine — that reveal what words don’t. The earlier you spot it, the faster you can help.
1. Watch the Face, Not Just the Words
Common Facial Expressions Linked to Pain
The face is a window into discomfort. Look for:
Grimacing or clenched jaw
Eyebrows pulled together
Rapid blinking
Sudden quietness or zoning out
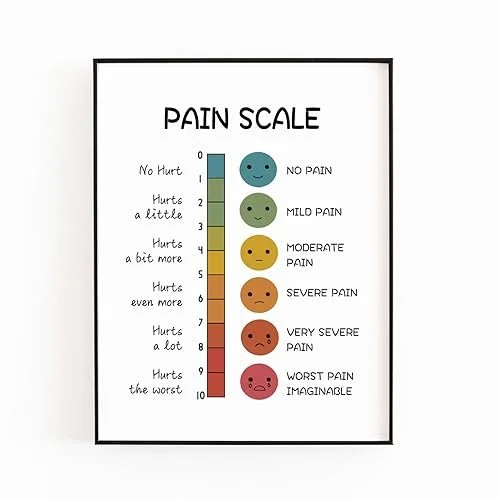
Tools Caregivers Can Use (Wong-Baker Scale)
One caregiver-friendly tool is the Wong-Baker Pain Scale — that row of smiley-to-crying faces you may have seen in clinics. For non-verbal loved ones (or those who minimize pain), it’s a simple, visual way to check in.
👉 Caregiver Pick: Wong-Baker Pain Scale Chart
2. Listen for the Sounds of Discomfort
Groans, Sighs, and Silence
Pain leaks out in sound — even if words don’t. Pay attention to:
Groans or moans when moving
Sharp intakes of breath
Sudden quietness in someone usually chatty
How to Keep a Simple “Pain Journal”
Patterns matter more than one-off moments. A quick “pain journal” in your phone’s notes app (time + what you heard/saw) can reveal trends — like pain worsening at night or after meals.
👉 Caregiver Pick: Notebook or digital pain journal
3. Body Language Tells the Truth
Guarding and Withdrawal Behaviors
If they’re holding or protecting a limb, belly, or back, that’s a red flag. Same goes for pulling away when you touch a certain area.
When Restlessness Speaks Volumes
Constant shifting in a chair, squirming in bed, or pacing can mean they just can’t get comfortable. Often, this is pain trying to find an outlet.
👉 Caregiver Pick: Pressure-relief cushions or mattress toppers
4. Spotting Changes in Daily Life
Eating, Sleeping, and Social Habits
Pain drains energy and interest. Look for:
Not finishing meals
Skipping hobbies or usual TV shows
Sleeping way more — or barely at all
Why Energy Shifts Can Mean Pain
If your loved one starts withdrawing from everyday activities, it may not be “laziness” — it could be their body screaming in ways they can’t describe.
5. Caregiver-Friendly Pain Relief Strategies
Hot and Cold Therapy Packs
Reusable gel packs are simple, affordable, and often more effective than people expect. Cold helps with swelling and fresh injuries; heat soothes stiffness and chronic aches.
Positioning and Support Cushions
A well-placed pillow can do wonders. Prop them up, wedge between knees, or roll a towel for lumbar support.
Safe Over-the-Counter Options
Some caregivers find relief using basic store-bought pain relievers, but the real key is making sure doses aren’t doubled up or missed. Keeping a simple medication log (notebook or printable chart) helps track timing and avoid mistakes — especially during long nights or when multiple caregivers are involved.
👉 Caregiver Pick: Medication tracking log or notebook
Distractions that Actually Work
TV, music, games, coloring books, or prayer — all can turn down the “volume knob” on pain by shifting focus.
6. When It’s Time to Call a Professional
Red Flags Caregivers Shouldn’t Ignore
Sudden, severe, or unexplained pain
Pain that worsens despite rest or basic measures
Pain paired with chest tightness, fever, or confusion
Encouraging Loved Ones to Speak Up
Remind them: saying “I’m in pain” isn’t complaining — it’s self-care. Sometimes framing it as “let’s keep you comfortable” works better than asking “are you in pain?”
7. Caregiving Isn’t About “No Pain” — It’s About “Manageable Pain”
You won’t eliminate every ache or twinge. The win is making pain manageable so your loved one can still eat, laugh, rest, and live life. That’s victory.
Recommended Caregiver Tools (Affiliate Picks)
Caregiving is hard enough. These tools can make it a little easier — for both you and your loved one.
Wong-Baker Pain Scale Chart 👉 Get it here
Pressure-Relief Cushions or Mattress Toppers 👉 Shop options here
Reusable Hot/Cold Gel Packs 👉 See caregiver favorites
Pain Journal or Notebook 👉 Grab one here
💡 Tip: You don’t need everything at once. Start with one tool that solves your biggest daily struggle, then build from there.
FAQs on Recognizing and Managing Pain
Q1: What are the most common signs of hidden pain?
Facial grimacing, withdrawal, restlessness, and changes in sleep or appetite are top signs.
Q2: How do I ask my loved one about pain without making them defensive?
Use open questions like “How’s your comfort today?” or offer the Wong-Baker scale.
Q3: Can pain get worse at night, and why?
Yes. At night there are fewer distractions, the body is still, and the mind fixates on discomfort.
Q4: What’s the difference between chronic and acute pain?
Acute pain is short-term and linked to injury/illness. Chronic pain lasts months or years, often persisting after healing.
Q5: When should I call a doctor about pain?
If it’s sudden, severe, worsening, or paired with fever, chest pain, or confusion, call right away.
Q6: Do non-medication options like heat/cold or distraction really help?
Yes — they won’t replace medical care, but they can lower pain levels and improve comfort.
Conclusion: Trust Your Gut, Not Just Their Words
At the end of the day, spotting pain isn’t about perfection — it’s about noticing the small signs, acting early, and giving your loved one comfort and dignity.
Remember: caregiving isn’t about chasing “no pain ever.” It’s about making pain manageable so your loved one can still laugh, eat, sleep, and enjoy life. That’s the real victory.
👉 If this post helped, you’ll find dozens more practical, unfiltered caregiving insights in my book:
The Unmedical Manual for Caregivers by James Adams
It’s the guide I’ve written for the caregiver whose had no prior training with no jargon, no judgment, and real-world caregiving wisdom you can actually use.
⚖️ Important Disclaimer
This article is for educational and caregiving support purposes only. It is not medical advice and should not replace professional evaluation, diagnosis, or treatment. Always consult a qualified healthcare provider regarding any medical concerns, new pain, or sudden changes in health.